Be the perfect patient? Whether you saw your primary doctor or an emergency room doctor, physicians like follow-up. This is most important if a problem does not clear up or returns. For example, if you head to the doctor with joint pain complaints and are treated with pain relievers and home therapies but the pain doesn’t resolve, you need to see your doctor again. There may be reason for additional tests or a more intense rest period, however there is no way to know that if you don’t call and inform the doctor of changes, or a lack thereof. What it comes down to is being your own advocate. Your doctor may be the medical expert, but you’re the you expert. You know you best and when something isn’t feeling right, calling the doctor to follow-up isn’t a nuisance, it’s a necessity. Sometimes doctors appointments offer little more than reassurance that the mole you’ve been stressing over for months is nothing to be afraid of, but in any case it’s a worthy use of your time.
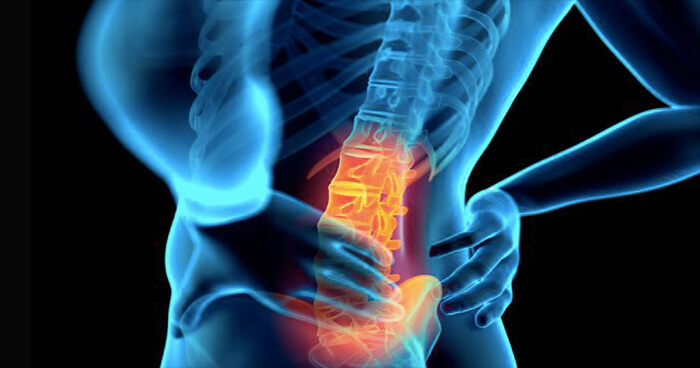
The most common cause of back pain ? There are three common types of nerve root issues that lead to back pain: spinal stenosis, spondylolisthesis and osteoarthritis. In all three conditions, the nerve root is affected causing often-severe back pain. In spinal stenosis the pain results from narrowing of the spinal canal near the nerve roots. It can appear in one area, or several areas, of the back. In spondylolisthesis, a vertebrae slips over another vertebrae and creates a painful, unstable back. Spondylolisthesis most commonly occurs with joint issues, typically after a fracture or a degenerative joint disease, or as the result of a defect to the joints. Lastly, osteoarthritis occurs when both discs and joints begin to wear down. This ailment becomes more common as people age and leads to pain, swelling, instability and stenosis in one or several areas of the spine.
Scoliosis is a medical condition in which the person’s spine curves sideways. This condition usually includes pain, uneven shoulders, and differing leg length. Adult scoliosis occurs when a person has reached spinal maturity. What is it scoliosis? Adult scoliosis is defined as a spinal deformity in a skeletally mature patient with a curvature of more than 10 degrees. When this curvature occurs, it can be accompanied by twisting or rotating of the spine as well, and the spine takes on the shape of an elongated “S”. Adult scoliosis can be classified into four major groups: Type 1- Primary degenerative scoliosis is caused by disc deterioration and/or facet joint arthritis. This condition causes back pain, and an asymmetrically change in the spinal column. Type 2- Idiopathic adolescent scoliosis that has progressed in adulthood. This may be the result of secondary degeneration and/or spinal imbalance, with or without a history of corrective spinal surgery. Type 3- Secondary adult curves a) resulting from a neuromuscular or joint abnormality causing a leg length discrepancy or hip pathology, or b) caused by metabolic bone disease (osteoporosis) combined with asymmetric arthritic disease and/or vertebral fractures. Patients that experience these symptoms predominantly complain of back pain, then leg pain and claudication symptoms (pain in the feet, calves, thighs, hips or buttocks with exercise) and numbness or tingling.
Dr. Yuan treats a range of spinal disorders in patients of all ages including herniated discs and stenosis in the cervical, thoracic and lumbar spine. Dr. Yuan never recommends surgery first and is a thought leader in managing degenerative spinal stenosis. Dr. Yuan is a board certified Orthopedic Surgeon and fellowship trained spinal surgeon. He specializes in the treatment of all spinal disorders including issues with the neck and back. He treats conditions that affect the cervical, thoracic and lumbar spine utilizing both surgical and non-surgical interventions. Dr. Yuan emphasizes non-surgical treatment first and only recommends surgical procedures when absolutely necessary to better a patient’s quality of life. Discover more details at Long Beach Spine Surgeon.
In some cases, surgery can be performed to reduce or eliminate SI joint pain. The two most common surgical approaches are SI joint stabilization and joint fusion, both of which are typically done after other therapies have failed. For the latter, minimally invasive Sacroiliac Joint Fusion systems has shown positive results in treating SI joint dysfunction. Individualized rehabilitation programs aim to treat the underlying cause of SI joint pain. By treating the underlying cause, the pain should subside and the runner can return to their routine with little modification. Sometimes bracing will be needed while a person heals. In cases where pain is severe, pain medication or steroid injections may be recommended to keep pain under control while the person rehabilitates, and when the dysfunction is very severe, surgical intervention may be required to eliminate pain and treat dysfunction and its underlying causes.